
Created by - Dr. Prashant Raj
Epilepsy – Affect Type & Disorder
Epilepsy is a neurological disorder that could lead to uncontrolled bursts of electrical activities owing to the improper functioning of nerve cells. This temporary uncontrolled burst or excessive surge of electrical activity within the brain is called a Seizure, which could give rise to symptoms depending on which part of the brain is affected. Epilepsy is a chronic disease that causes repeated seizures, usually when someone experiences 2 or more unprovoked seizures within 24 hours. twenty-four hours apart. “Unprovoked” seizures are those that aren't brought on by a usual cause, like alcohol withdrawal, heart issues, or hypoglycemia, that is once someone has extraordinarily low glucose levels. Seizures are also the results of change in normal biology or a brain injury, however, typically their cause is unknown. The words “seizure disorder” and “epilepsy” are typically used interchangeably. Types of seizure - There are 2 main sorts of seizures—Focal, which are referred to as partial seizures, and generalized. Focal seizures begin with abnormal discharge restricted to at least one tiny region of the brain. Affects one area of the brain and stays confined to 1 hemisphere. Symptoms will embody altered behaviors, thoughts, or movements. Causes: o Focal seizures are also caused by an associated underlying structural abnormality within the brain. o Focal seizures may result to go trauma, stroke, infection, tumors, or different causes. o Certain genetic disorders may cause focal seizures. Types of Focal SeizuresFocal seizures are of 2 types1. Simple focal seizures or Focal aware seizures: When a person is conscious and fully aware of what is happening2. Complex Focal seizures or Focal impaired-awareness seizure: Consciousness is usually affected and awareness is disrupted, and you will not be aware of what is happening around you. Generalized seizures begin with a widespread, excessive discharge involving each hemisphere, or side, of the brain. Symptoms embody staring and blinking, jerking movements, loss of tone, and stiffening of limbs. once the whole brain is involved, symptoms include regular, full-body jerking. Seizures that arise from each hemisphere of the brain at the same time and spreads over The reason for generalized seizures is likely to be genetic. Very seldom is the disorder inherited disorder and typically it's an unknown cause. Difference Between Epilepsy and Seizure -Understanding the distinction between seizures and brain disorder starts with knowing seizures constitute 2 main classes counting on why they happen. o Provoked seizures: These happen attributable to different conditions or circumstances (high fevers, alcohol or ending, low blood sugar). These seizures constitute 25% to 50% of all seizures.o Unprovoked seizures: These are not symptoms of a current medical condition or circumstance and occur once a person’s brain will cause spontaneous seizures. This conjointly includes seizures that happen after 7 days when a particular cause (like a head injury or stroke) had occurred.Epilepsy could be a brain condition that puts you in danger of getting spontaneous, unprovoked seizures. Health care suppliers diagnose it after you have a minimum of 2 unprovoked seizures, Or you have one unprovoked seizure and have a high risk of getting a minimum of a new one within the next ten years. Having one unprovoked seizure will increase the chances of getting another. How does it affect our body?Your brain contains billions of cells called neurons. These cells transmit and relay chemical and electrical signals. One nerve cell in your brain connects to thousands of additional, forming human neural activity networks. Those networks of your brain work along so that you'll be able to do things like solve issues, store recollections and move around. Seizures happen once a malfunction causes neurons to fire electrical signals uncontrollably. That causes neurons to go haywire. The more haywire neurons, the larger the impact of the seizure. If these malfunctions happen more often, it will affect how your brain cells work and cause seizures to happen. If they keep happening or seizures last too long, these electrical malfunctions can harm and destroy your brain cells. once this happens to enough neurons in a part of your brain, the result may be permanent brain damage. Seizures may cause severe changes in your blood chemistry as your body tries to manage the physical effects of convulsions. Causes of Seizure - Seizures will happen for several different reasons. These include: o Aneurysms.o Brain tumors o Cerebral hypoxia (lack of oxygen).o Severe concussion and traumatic brain injury.o Degenerative brain disorders like Alzheimer’s disease o Drugs and alcohol (this includes prescription medications, recreational medicine, and even caffeine).o Drug or alcohol withdrawal.o Eclampsiao Electrolyte issues, particularly low sodium (hyponatremia).o Fevers, particularly high ones o Genetic disorders (conditions you've got at birth that you just transmissible from one or both parents).
More detailsPublished - Sat, 13 Aug 2022

Created by - Dr. Prashant Raj
Save your skin from scorching sun
Summers mark a begin of the style season. In apparels, nothing will beat the warmth the maximum amount as short floral dresses, skirts, capris, etc. Everyone likes to wear comfy ethereal garments as they not solely invigorate your mood however conjointly give a reprieve from sweltry weather. Summer is here and with it comes additional outside activities and travel. Not with standing your plans this summer, there square measure some safety precautions that each one families ought to remember of. 1) As they are saying precaution is usually higher than cure, thus avoid going call at the sun once its heating intensity is at peak i.e. between midday and three pm. 2) Wear sun screen on your exposed body elements, or opt for a lotion that has a minimum of 20+ spf. Slathering UVA & UVB obstruction sun screen prevents sun burn and sun tan. Fingers and toes square measure the foremost unnoticed areas thus bear in mind to use sun screen in between toes and fingers still. 3) If you have got to remain within the sun for long hours then make sure that you're sporting full gloves and socks so as to guard your hands and feet from sun burns severally. 4) Invariably carry associate degree umbrella with you. Umbrellas aren't speculated to defend you from rain solely, however sun still. 5) Flip flops and strap sandals square measure summer favorite – however they supply marginal protection from sun. Always, make sure that your wear such footwear that has full coverage to your feet, and therefore protection from hot summer.
More detailsPublished - Tue, 16 Aug 2022

Created by - Dr. Prashant Raj
Orthopedic emergencies and its types
Orthopedic emergencies are sudden medical conditions involving the spine, the limbs, or related structures, or involving their aberrant shape or function. Orthopedic emergencies are frequent in the emergency room (ED) and can pose a risk to limb function if not handled immediately.TYPES OF ORTHOPEDIC EMERGENCIES1. Muscle contusion (bruise): A muscle contusion is caused by blood extravasating into the muscle tissue as a result of direct stress. At first, the bruised muscle will be tender and swollen, and the skin above it will seem red or blue (ecchymosis). The hue of the skin shifts from purple to a greenish-yellow as the blood is reabsorbed.2. Strain: The degree of muscle fiber damage that develops after a muscle is either too stretched or violently flexed against resistance is used to categorize muscular strain injuries.a) First-degree muscle strain is a minor stretching injury of the muscle fibers that is characterized by muscle spasm, mild swelling, local tenderness, and a slight decrease in function.b) Second-degree muscle strain is a partial tearing of the muscle fibers that is characterized by moderate swelling, ecchymosis, and decreased functional strength.c) Third-degree muscle strain is a complete disruption of the muscle that is characterized by swelling, ecchymosis, decreased strength, and a palpable “bulge” caused by the retracted unattached muscle belly. Third-degree muscle strains can lead to significant long-term disability but fortunately are not as common as first- and second-degree strains.3. Sprain: Sprains are damage to the ligaments in the joints that happen when a joint is forced to move abnormally.a) First-degree sprains are characterized by mild hemorrhage and swelling, minimal point tenderness, and no abnormal joint motion (i.e., the joint is stable).b) Second-degree sprains, which occur when the ligaments are partially torn, result in moderate hemorrhage and swelling, tenderness, painful motion, loss of function, and minor joint laxity.c) Third-degree sprains occur when the joint ligaments are completely disrupted. Third-degree sprains may initially appear similar to second-degree sprains, but the patient will have severe joint instability after the swelling subsides.4. Dislocation: When the opposing articular surfaces of the bones are no longer in touch, a joint is said to be dislocated. A partial dislocation is a subluxation (i.e., the articular surfaces are in partial contact).5. Fracture: The disruption of the bony cortex results in a fracture. Pain, edema, and deformity are brought on by the bleeding into the surrounding tissue from the broken bone.a) Descriptive terms: Important details include the following: the affected bone, fracture location, whether the fracture is open or closed, whether the intra-articular extension has occurred, the type of fracture line, description of bone fragments (if present), whether the fracture is complete or incomplete, neurovascular status, and the position or alignment of the bone segments.An open fracture occurs when the skin overlying the fracture is not intact either due to direct trauma or a fragment of bone that penetrates the skin. A subtle open fracture can occur when a bone fragment pierces the skin and then withdraws, leaving only a small puncture wound. Therefore, any fracture with an overlying skin wound should be suspected of being open. A closed fracture occurs when the skin and soft tissue overlying the fracture are intact.An intra-articular fracture is a fracture that extends into the joint surfaces.The fracture line may be spiral, oblique, or transverse. Fractures in children are often described as the buckle (torus), greenstick, or complete fractures. A fracture can also be described as compression, avulsion (chip), or comminuted (shattered) fracture.The bone segments may be in contact with each other or separated by a measurable distance (usually stated in millimeters). The bone segments may be completely displaced (i.e., lying next to each other instead of end to end), partially displaced (i.e., offset from each other by a measured amount), or non-displaced.The angulation of the two bone segments is described by both the direction of the angle (e.g., radial, dorsal, anterior, lateral) and by the degree of the angle formed by the two bone segments.b) Special fracturesPathologic fractures occur when a relatively minor force is applied to the diseased or otherwise weakened bone.Stress fractures are caused by the repetitive application of a minor force to a bone, usually a long bone in the lower extremities. Stress fractures are commonly seen in military personnel (march fracture) and athletes (e.g., joggers, dancers).Salter-Harris fractures involve the epiphyseal plate (i.e., the growth plate) and are common in children.
More detailsPublished - Wed, 17 Aug 2022

Created by - Dr. Prashant Raj
How to Diagnose Orthopedic Emergencies
A comprehensive physical examination and careful consideration of the patient's medical history can identify many orthopedic emergencies. The emergency doctor takes the patient's medical history and completes a physical examination to determine the potential type and severity of the injury before selecting the best radiography image to confirm the probable diagnosis.PATIENT HISTORY1. Patient age: The patient’s age may give some indication of the type of injury, (e.g., Salter-Harris fractures only occur in young patients, whereas hip fractures are more common in the elderly).2. Chief complaint: Patients with orthopedic emergencies typically present with one or more of the following complaints: pain, swelling, redness, deformity, or diminished function.3. Mechanism of injurya) To forecast the type of injury, it is crucial to understand the mechanism of injury (i.e., how the injury happened). For instance, it could be challenging for a doctor to make a diagnosis in a young child with normal radiographs who won't use his or her right arm if they don't understand the mechanism of the damage. However, the likely diagnosis (radial head subluxation) becomes immediately clear if the doctor is aware that the infant has just been pulled by that arm.b) Selecting the appropriate radiographic images is aided by understanding the cause of damage, particularly when the patient is uncooperative, experiencing transferred pain, or has a distracting injury. For instance, a patient with acute shoulder pain following an injury might get a routine, ordinary shoulder radiograph. However, a second examination of the shoulder can be acquired to confirm this diagnosis if the cause of injury points to posterior dislocation.4. Preexisting illnesses or conditions: The physician should inquire about illnesses and conditions that may negatively impact the healing process (e.g., diabetes, heart disease, steroid therapy, and cancer chemotherapy).PHYSICAL EXAMINATION1. Inspection: The suspected area of injury should be inspected for swelling, discoloration, deformity, abrasions, puncture wounds, and lacerations.a) Orthopedic injuries (including fractures) may have few or no obvious visible abnormalities, especially in children.b) Muscle contusions and severe sprains may result in localized swelling that is similar to the swelling seen with fractures. Radiographs are frequently needed to differentiate sprains and fractures.2. Palpation of the entire extremity may reveal point tenderness, subtle deformities (e.g., a “step off”), or bony crepitus. The area distal and proximal to the pain location should be systematically palpated. Complete palpation is important for two reasons:a) The patient may be unaware of a second injury because of the pain of the primary injury.b) If radiographs are ordered before complete palpation, radiographs of the correct bone may not be obtained.3. Range of motion assessment: Each joint near and far from the injury should, wherever practical, be examined for passive and active range of motion. It is important to record the degree of flexion, extension, and discomfort. To identify small anomalies, the contralateral (unaffected) joint may need to undergo a second assessment of the joint's function.4. Neurologic examination: Nerve injury can result in either sensory or motor deficits. Sensation distal to the injury should be identified before any manipulation of the extremity takes place. Muscles that are innervated by the major nerves of the extremity should be examined for motor function.5. Arterial blood flow assessment: Some orthopedic emergencies (e.g., knee dislocation, fracture or dislocation of the ankle, supracondylar fracture of the elbow in children) are commonly associated with vascular (arterial) injuries. The earlier circulatory compromise is identified and addressed, the less likely it is that permanent injury will result.RADIOGRAPHY1. Viewsa) Standard: The area to be examined radiographically should be based on the history and physical examination findings. Frequently, imaging the joint above and the joint below a suspected fracture is indicated to detect associated fractures or dislocations. Most extremity radiographs include an anteroposterior view, a lateral view, and an oblique view.b) Special: Some fractures are only visible using special radiographic views. Some common orthopedic emergencies that require special views include acromioclavicular separation, fracture of the carpal navicular, posterior shoulder dislocation, and sternoclavicular dislocation. Children may need comparison views of the unaffected extremity to detect epiphyseal plate injuries.2. Findingsa) In the case of stress fractures, the initial radiographs may be normal. However, the presence of new bone growth or bone resorption (which causes the fracture line to become visible) on radiographs taken 2 to 3 weeks later may suggest the fracture. If a fracture is highly suspected but the radiograph is normal, treatment for the fracture should be initiated.b) The normal growth plate appears as a transverse, radiolucent line at the end of the bone. The growth plate can be easily confused with a transverse fracture.
More detailsPublished - Wed, 17 Aug 2022

Created by - Dr. Prashant Raj
What is choking? Causes of choking, Important Steps, Heimlich Maneuver.
Children typically choke from inserting objects in their mouths. They usually try this out of curiosity. However, they'll start choking immediately after ingestion, too quickly Common objects that youngsters choke on are:PopcornCandyPencil erasersCarrotsHot dogsChewing gumPeanutsCherry tomatoesWhole grapesA large piece of fruitA large piece of vegetablesAdults typically choke while swallowing food if it's not chewed properly or you are eating in a hurry or while laughing/talking. What to do if somebody is choking?Use the Red Cross’ “five-and-five” methodology to treat someone who’s choking: Hit the person’s back with the heel of your hand 5 times between the shoulder blades. Next, perform the Heimlich maneuver 5 times. Alternate between the 2 till the person is no longer choking.Don’t perform the five-and-five methodology on a toddler. You must solely provide a kid with the Heimlich maneuver.The Heimlich maneuver - Follow these steps to perform the Heimlich maneuver:Stand behind the person together with your arms wrapped around their waist.Lean the person forward.Ball your hand into a hand and place it on the person’s abdomen, on top of their navel.Grip your hand and press into the person’s abdomen in an upward motion.Repeat this methodology 5 times.If the thing continues to be stuck within the person’s throat, repeat these steps 5 additional times.If the person is unconscious, clear their airway if possible with your finger. However, be cautious to not push the thing more deep into the throat. Visit your doctor afterward for further advice.
More detailsPublished - Wed, 17 Aug 2022

Created by - Dr. Prashant Raj
Frostbite – Risk, Stage & Symptoms
Frostbite is common however it is usually underestimated condition wherein your skin gets affected after exposure to extreme cold weather conditions or cold water. The symptoms include swelling, blisters, and blackened skin. Whereas winter weather is fun, it may also be dangerous. Frostbite can lead to a permanent issue that happens once your body tissues (like fingers, toes, and ears) are scraped by exposure to weather conditions or cold water. This usually happens during extreme chilling winter, in windy weather, and at high altitudes. Who is at risk of developing frostbite?If your skin is exposed to cold temperatures, you’re in danger of hurt. You’re additionally at a higher risk of developing frostbite if you:• Have chronic disease.• Smoke.• Have peripheral artery disease • Have Raynaud’s disease, a condition that involves periodic narrowing (or spasms) of the blood vessels.• Have poor blood circulation or dehydration.• Haven’t dressed befittingly for weather conditions or high altitude (swimming, hiking, or climbing).• Are elderly• Have a physical or mental condition that stops you from protecting yourself against the cold• Have been drinking alcohol. What are the three stages of frostbite?Frostbite begins with delicate symptoms that may develop quickly after exposure posing a high health risk if the exposure is longer. There are 3 stages including:· Frostnip is a mild type of frostbite, where the skin is red or a pale white. The skin may additionally feel cold, numb, or tingly. Frostnip is the warning stage when the symptoms remain simply temporary. Thus if you notice symptoms get within forthwith and treat the lesion with heat (never hot) water.· Superficial (surface) frostbite: This is the second stage where water under the skin may change the phase to ice crystals, and the skin may swell. you may see dappled patches or purple or blue areas that hurt or burn (just sort of a bruise). Your red skin would possibly begin to peel and hurt just like sunburn — and at this point, you may need immediate medical treatment. You may get fluid-filled blisters within a day too. · Severe (deep) frostbite: In the third stage of deep frostbite all layers of the skin and underlying tissues are affected. The skin changes its color from healthy pink to pale white or blue-gray. The area becomes completely numb, and all sensations of cold, or pain are lost. The movement is lost as Joints or muscles may completely stop working. After rewarming, Large blisters are formed after 24 to 48 hours. The tissue dies as it becomes hardened and may need to be removed surgically. Symptoms of Frostbite–Frostbite becomes severe as your skin temperature drops or the longer your skin stays exposed. The symptoms include:• Numbness.• A painful feeling of “pins and needles” within the exposed space.• Hardening of your skin that’s been uncovered for too long in the cold.• Redness (for delicate frostbite).• Pale or waxy (for severe frostbite).• Swelling.• Blisters (clear or blood-filled) or scabs. • Loss of coordination (stiff movements, falling).
More detailsPublished - Thu, 18 Aug 2022

Created by - Dr. Prashant Raj
Basic management of orthopedic emergencies
1. Sprains: Since ligaments don't have a lot of blood flow, sprains can take up to 8 weeks to heal. Dismissing the injury as "just a sprain" should be avoided by doctors because doing so gives the patient the unreasonable expectation of a quick and complete recovery.a) First and second-degree sprains: RICE, which stands for rest, immobilization, compression, and elevation, is the first line of treatment, along with analgesics or anti-inflammatory drugs. Typically, first- and second-degree sprains don't have any lasting effects.b) Third-degree sprains: Patients with third-degree sprains should seek immediate orthopedic advice since these injuries might result in permanently reduced joint function. For several weeks, these sprains may need to be immobilized in circumferential casts, or they may need to be surgically repaired.2. Fractures and dislocationsa) Stabilization of the patient: Although orthopedic emergencies are seldom life-threatening, concurrent life-threatening injuries may be present. Therefore, airway, breathing, and circulation (the ABCs) should be assessed first and appropriate measures are taken. Generally, in multiple trauma patients, airway, head, thorax, and abdominal injuries are treated before orthopedic injuries, although some orthopedic injuries (e.g., pelvic fractures of midshaft femur fracture) can significantly contribute to hemodynamic instability.b) Reduction of swelling: Swelling occurs early after a fracture or dislocation and can increase the patient’s pain and delay the application of definitive immobilization.— Elevation of the extremity and application of cold compresses are effective measures for preventing the progression of swelling.— Potentially constricting jewelry on the injured extremity should be removed in anticipation of extremity swelling.c) Temporary immobilization: The suspected fracture or dislocation should be immobilized early in the ED visit. Immobilization reduces the patient’s pain, diminishes the potential for damage to the neurovascular bundle, and reduces swelling and bleeding. Additionally, stabilization and immobilization facilitate patient transport, expedites the radiographic examination, and, in the case of fractures, reduce the chance of a sharp bone fragment puncturing the skin and converting a closed fracture to an open fracture.— For fractures, temporary immobilization is accomplished by splinting across the fracture and the joints proximal and distal to the fracture.— For dislocations, the joint may be immobilized using a splint or sling.d) Pain control: Most patients with fractures or dislocations will become increasingly comfortable when the extremity is sufficiently immobilized.e) Reduction is the process of restoring the bone or joint to its normal anatomic configuration: Early reduction decreases pain, may restore circulatory or nerve function, and prevents the progression of swelling.— Generally, a radiograph of the bone or joint is obtained before the reduction of the fracture or dislocation.— Analgesics and sedatives are usually required for most reductions, which are generally accomplished by applying slow, steady, longitudinal traction.— A post-reduction radiograph is always needed to document the success of the procedure, determine if additional injuries are present, and assess the need for additional treatment.f) Post-reduction immobilization: Reduced fractures and reduced dislocations must be immobilized before the patient is released from the ED (see Immobilization). Immobilization1. Splints or circumferential casts are usually used to immobilize fractures: Splinting is less likely than circumferential casting to lead to pressure sores, circulatory compromise, and neurapraxia. After the swelling has decreased, a circumferential cast can be applied.a) Patients with fractures that are not prone to complications and have only minimal swelling may be treated in the ED with circumferential casting.b) Splints are usually made from plaster of Paris or fiberglass. Water causes an exothermic chemical reaction, which causes the material to harden over several minutes. During this process, the splint is molded along one side of the extremity, which is held in the appropriate position. Padding is placed between the skin and splint, and the splint is secured to the extremity with an elastic bandage wrapped circumferentially around the extremity and splint.2. Immobilization dressings: In addition to splints, several dressings are commonly used in the ED. Examples include the shoulder sling, sling and swath, and knee immobilizer.
More detailsPublished - Fri, 19 Aug 2022

Created by - Dr. Prashant Raj
How to diagnose Frostbite? What are the Causes and Treatment
Causes –o Frostbite happens when skin is exposed to cold temperature or cold water for an extended time o Direct contact with Ice packs and cold metal may also cause harm if they’re ironed directly against your skin. The water in the skin freezes due to cold exposure which may cause visible and invisible harm to cells and soft tissues. It usually affects extremities [fingers/ toes/ears], however, it can also affect the cheeks and chin. The damage can go deep below the skin, including muscles, nerves, and jointsDiagnosisThere are not any easy tests to inform how badly you’ve been impacted by frostbite. The physician will inspect the area, and evaluate the history of cold exposure that including the time, the person was exposed to extreme temperatures. o Depending on the stages of frostbite and associated symptoms imaging methods [such as X-RAY] can be used to diagnose the severity.o Physical examination may include inspection of skin color [white/red/black] and presence of blisters [clear or blood-filled]. o Clear blisters indicate temporary damage whereas blood-filled blisters are suggestive of long-term damage. o Black gangrenous skin needs surgical removal for preventing gangrene. TreatmentTime is vital when you are exposed to severe cold and experience symptoms of frostbite such as pain or red fingers. Immediately move into the warm area and gently heat your skin. If symptoms are severe [2nd/3rd stage] then seek emergency medical care immediately too Help raise your blood temperatures in lukewarm water or by applying heat for half an hour.o Dress your frozen or wounded skin with sterile bandageso Keep your fingers and toes separated to avoid rubbing.o Test blood flow in the affected area. In the case of 3rd stage frostbite, blood circulation and hydration can be improved by giving IV fluids. o Antibiotics, pain relievers, tetanus shots, and/or oxygen therapy are given as supportive therapy
More detailsPublished - Sat, 20 Aug 2022

Created by - Dr. Prashant Raj
Impact of Epilepsy on quality of life?
The impact of epilepsy is varied and intensive. The incidence of seizures is unpredictable and infrequently dangerous, increasing the danger of injury, hospitalization, and mortality. It also adversely affects a patient's psychological state, usually leading to anxiety, depression, or psychological impairment. Seizures may end in social exclusion, with harmful effects on self-confidence. However, the burden of the disease extends more as compared with the consequences of seizures themselves. The side effects of medicines and the disease itself invariably have been shown to impact negatively on subjective health and quality of life.Patient surveys give valuable insights into what matters to patients in their daily lives and highlight necessary discrepancies between the perceptions of patients and their physicians. for instance, survey information shows that physicians underestimate the number of patients experiencing medicine-related side effects and also the impact of those on patients. Screening questionnaires facilitate physicians to quickly determine issues with treatment side-effects and effects; conjointly, to acknowledge comorbidities like depression that might be difficult to spot in a time-limited consultation. Ultimately, it is certain that epilepsy needs a holistic approach, with treatment tailored to the individual patient's needs; this could solely be achieved through effective doctor-patient communication and also the full involvement of a multidisciplinary care team.Epilepsy may be a varied chronic disorder that has various and complicated effects on the well-being of the patient. Though it's evident that seizure duration and frequency play a crucial role in the quality of life (QOL) of patients with the disease, it's less clear what are the key determinants that influence QOL in patients receiving therapy.Home Safety measures needed to be taken for the patient with Epilepsy -Many flats or homes should be modified to create safe environments for folks that have seizures. Several of those changes are straightforward and don't need a lot of time or investment. If vital changes are necessary, make sure to contact the owner or property manager before creating the changes. These straightforward fixes may result in an exceedingly vital increase in safety:First, Walk-through the rooms to identify potential dangers. Note any sharp corners on a piece of furniture and counters, slippery floors, or hot places like fireplaces and stoves. Also, places with staircases and pools have distinctive issues.General Precautions– All the floors of all rooms should be covered with dense pile carpet to safeguard from falling injuries. Also, pad any sharp corners which can hit while falling during a seizure. Make sure that every walkway is free from obstacles.The Kitchen– Use appliances that can shut off mechanically once not in use. Try to use a kitchen appliance rather than a stove for cookery. If you're employing a stove try to use electrical over gas, to avoid the burns if a seizure happens. Plastic containers should be substituted for glass which can shatter and may cause hurt The lavatory– Bathroom doors ought to open outward, not inward just in case seizures occur in the restroom. Install a shower seat, non-slip strips, and grab bars within the bathroom. Use glass for shower doors. Be aware of water temperature settings. Keep the bath drain flowing freely and keep tub water levels low.Living Alone–Use a “buddy system” and have somebody decide for you if you are not well. Pre-program necessary phone numbers. take a private care hotline like Lifeline just in case of emergency. Keep floors clean from litter. Place barriers ahead of any things which will get hot like stoves and radiators. Have chairs that have arms that are often a little low to stay safe throughout a seizure. The challenges of living with epilepsy are also completely different for kids, adolescents, and seniors.
More detailsPublished - Thu, 25 Aug 2022
Search
Popular categories
Latest blogs
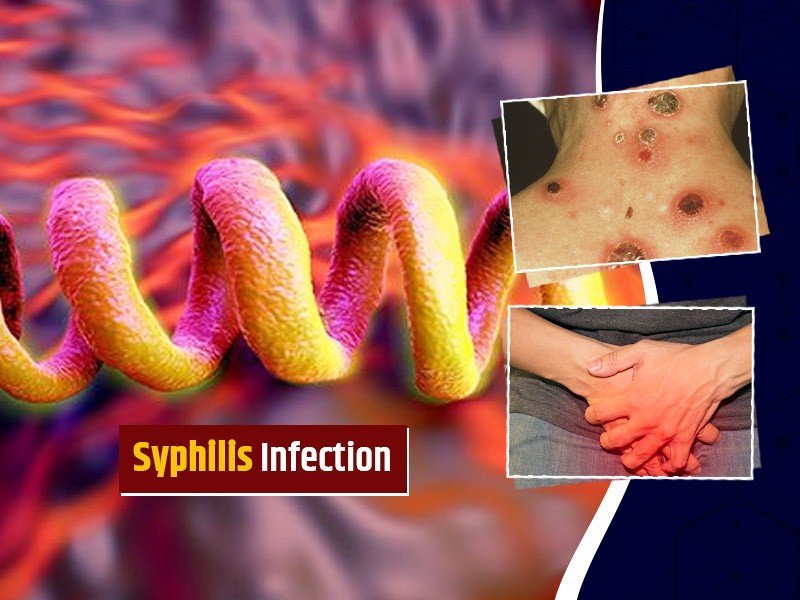
All you need to know about Syphilis
Tue, 15 Nov 2022
What is Pemphigus Vulgaris?
Tue, 15 Nov 2022

Know about Scorpion Stings
Sat, 12 Nov 2022
Write a public review