Published - Wed, 19 Oct 2022

Noncardiogenic pneumonic edema
Noncardiogenic
pulmonary oedema is an illness that leads to acute hypoxia secondary to a fast
deterioration in respiratory function. The illness has multiple etiologies, all
of that need prompt recognition and intervention.
The
permeability of the alveolar-capillary membrane is increased which leads to the
increased leak of protein and water in the alveolar space causing an increase of
intra-alveolar fluid, thereby increasing pulmonary vascular resistance,
intrapulmonary shunt, and hypoxemia. This will cause a marked reduction in
compliance of Lung.
To
differentiate from cardiogenic pulmonary oedema, pneumonic capillary wedge
pressure isn't elevated. This is often necessary to differentiate because the
management of both conditions is different.
Pulmonary
oedema that's not caused by hyperbolic pressures within the heart is termed
noncardiogenic pneumonic oedema.
Causes of noncardiogenic Pulmonary oedema include:
o Acute respiratory distress syndrome (ARDS). This serious disorder happens once the lungs suddenly fill with fluid. several conditions will cause respiratory illness, as well as severe injury (trauma), and widespread infection (sepsis), respiratory illness.
o Drug reactions or side effects of several medications — starting from acetylsalicylic acid to medication like opiate and cocaine — are best known to cause pulmonary oedema.
o Blood clot in the lungs (pulmonary embolism). A clot moving from the blood vessels of the legs to the lungs can cause pulmonary oedema.
o Exposure to some toxins. Exposure to some toxins or aspirating some refluxed abdomen contents may cause intense irritation of the tiny airways and air sacs, leading to fluid build-up.
o High altitudes. Pulmonary oedema has been seen in mountain climbers, skiers, hikers and others who trip high elevations, typically around 8,000 feet. High altitude Pulmonary oedema (HAPE) typically happens in those that do not take the times or weeks necessary to become accustomed to the elevation. however, people that live at high altitudes will get HAPE with no elevation amendment if they need a respiratory disorder.
o Near drowning episodes in water can cause fluid build-up within the lungs.
o Negative pressure Pulmonary oedema. A blocked higher airway causes negative pressure within the lungs from attempting to breathe through the blockage. With treatment, most patients recover within 24 hrs with this type of Pulmonary oedema.
o Nervous system conditions or surgeries. Pulmonary oedema occurs after a head injury, seizure or surgery.
o Smoke inhalation. Smoke from certain chemicals can harm the membrane between the air sacs and also the capillaries. This harm permits fluid to enter the lungs.
o Transfusion-related respiratory organ injury. Blood transfusions might cause fluid overload resulting in Pulmonary oedema.
o Viral
sicknesses. Viruses like the hantavirus can cause Pulmonary
oedema.
Created by
Comments (0)
Search
Popular categories
Latest blogs
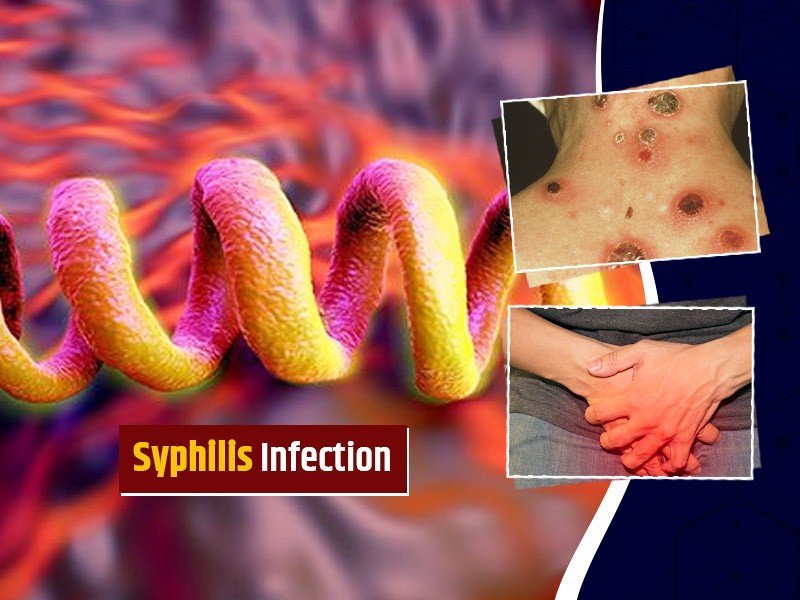
All you need to know about Syphilis
Tue, 15 Nov 2022
What is Pemphigus Vulgaris?
Tue, 15 Nov 2022

Know about Scorpion Stings
Sat, 12 Nov 2022

Write a public review