Published - Sun, 12 Jun 2022
What is Ramsay Hunt Syndrome? Causes, Risk, Complications & Symptoms
Ramsay Hunt syndrome (herpes zoster oticus) happens when the shingle affects the facial nerve close to one of your ears. Additionally to the painful shingles rash, Ramsay Hunt syndrome will cause facial dysfunction and deafness within the affected ear.
Ramsay Hunt syndrome is caused by a virus that causes chicken pox. Once pox clears up, the virus still lives in your nerves and may activate later to affect the facial nerve.
James Ramsey Hunt first described three discrete syndromes, the best known of which is herpes zoster oticus, also known as Ramsay Hunt syndrome type 2.
Ramsay Hunt syndrome Type 1, conjointly known as Ramsay Hunt neural structure syndrome, could be a rare kind of neural structure degeneration that involves myoclonic encephalopathy, progressive motor ataxia, and tremor.
Ramsay Hunt syndrome type 2, is the reactivation of herpes shingles within the neural structure. It is generally known as herpes shingles oticus, and has variable presentation which can embrace a lower neuron lesion of the facial nerve, deafness, vertigo, and pain.
Ramsay Hunt syndrome type 3 could be a less unremarkably documented condition, An occupationally induced pathology of the deep area branch of the cubital nerve.
Symptoms
The two main symptoms of Ramsay Hunt syndrome are:
A painful red rash with fluid-filled blisters on, in around one ear.
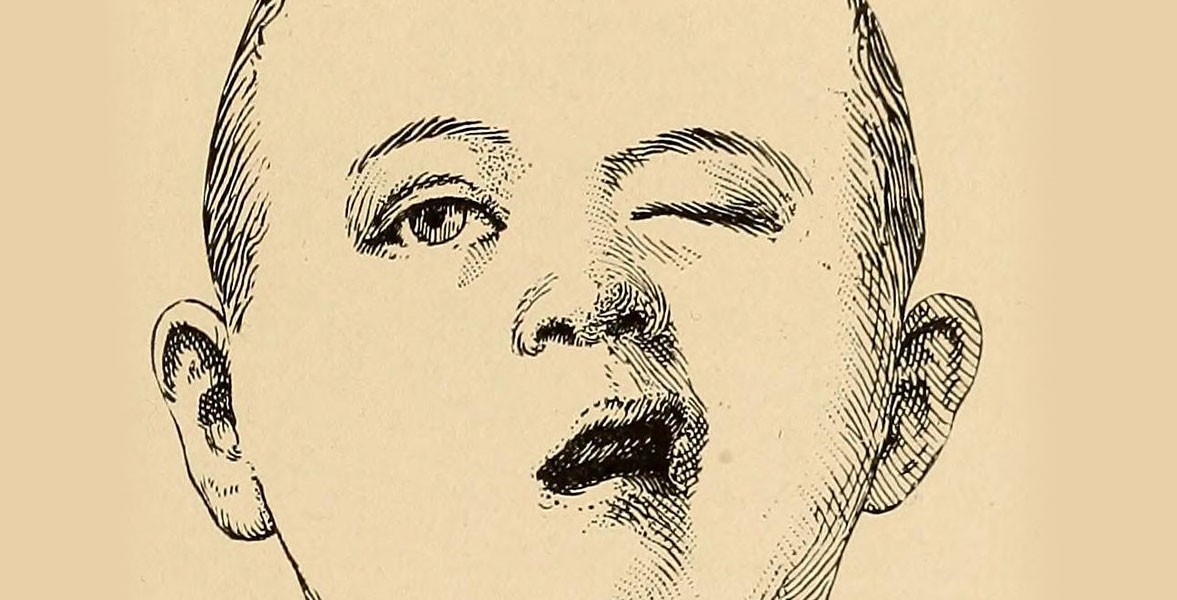
Facial weakness or disfunction on side of the affected ear
Usually, the rash and the facial dysfunction occur at the same time. If you've got Ramsay Hunt syndrome, you may also experience:
Ear pain
Hearing loss
Ringing in your ears (tinnitus)
Difficulty closing one eye
A sensation of spinning or moving (vertigo)
A modification in gustatory perception or loss of style
Dry mouth and eyes.
Causes
Ramsay Hunt syndrome happens in people who've had chickenpox. Once chickenpox clears up, the virus stays in your body, generally reactivating in later years to cause shingles, a painful rash with fluid-filled blisters.
Risk factors
It's common in older adults, especially older than sixty. Ramsay Hunt syndrome is rare in kids.
The infection may be serious for those who have low immunity.
Ramsay Hunt syndrome is not contagious. However, it is advisable to avoid contact until the rash blisters scab over, especially with
Anyone who's never had pox or who's never had the pox immunogenic.
Anyone who has a weak immune system.
Newborns.
Pregnant women
Complications
Complications of Ramsay Hunt syndrome may include:-
Permanent deafness and facial weakness: For many people, the deafness and facial dysfunction related to Ramsay Hunt syndrome are temporary. However, it may become permanent in a few cases
Eye injury: The facial weakness caused by Ramsay Hunt syndrome makes it difficult to close the eye, Once this happens, the cornea, that protects your eye, may get injured which may cause eye pain and blurred vision.
Postherpetic pain: This painful condition happens once a shingles infection damages nerve fibers. The messages sent by these nerve fibers become confused and exaggerated, inflicting pain that may last long even after signs and symptoms of Ramsay Hunt syndrome have reduced
Prevention
Children should be vaccinated regularly against pox, which greatly reduces the probability of getting infected with the pox virus.
Varicella vaccination is also recommended for people with age fifty or older
Call your doctor if you experience a facial dysfunction or a shingles rash on your face.
Created by
Comments (0)
Search
Popular categories
Latest blogs

All you need to know about Syphilis
Tue, 15 Nov 2022

What is Pemphigus Vulgaris?
Tue, 15 Nov 2022

Know about Scorpion Stings
Sat, 12 Nov 2022

Write a public review