
Created by - Dr. Prashant Raj
How am I able to cut back my Blood Pressure?
Everyone will enjoy taking measures to lower pressure levels. Even though you've got a healthy pressure level, you'll still try to take steps to make sure it remains healthy. The following modifications will help you to lower your blood pressure:Maintain a healthy weightStop smokingReduce salt intakeDrink alcohol moderatelyIncrease fruit and vegetablesStay physically activeTry to manage stressMaintain a healthy weightIt is well researched that being overweight is associated with an exaggerated risk of high-pressure levels. Maintaining a good diet will significantly cut back your pressure level. Losing as very little as 10% of excess weight will lower pressure levels. Being overweight is additionally a risk for cardiovascular disease and chronic disorders. Consult with your nutritionist/dietician to line realistic realizable goals for weight reduction. 10% weight reduction will lower your BP by 10-20mmHg.2. Stop SmokingIf you smoke, stop! Smoking is another major risk issue for cardiovascular disease and stroke. Once you quit, your risk of getting a heart attack is halved at intervals of 2 years. There are many different ways for quitting smoking/deaddiction. Consult your Doctor to check what's appropriate for you.3. Cut back your salt intakeIf everybody reduced salt intake and restrict it to 2.4 grams per day, this might stop roughly 900 deaths every year from stroke and cardiovascular disease. An excessive amount of salt consumption is directly connected to high blood pressure levels. Tips for thinning out your salt intakeDo not add salt to your food at the table.Cut down on processed foods that are typically high in salt.Try to season your foods with pepper, spices, or herbs as alternatives to salt.4. Eat a balanced diet rich in fruits and vegetables High-pressure levels are often reduced by following a healthy diet that's high in fruit and vegetables. Adults are supposed to take at least five servings of fruit and vegetables daily. Consume many colorful seasonal fruit and vegetables as they are considered to prevent diseases like cardiovascular disease and stroke.5. Drink alcohol sparselyExcessive alcohol consumption is associated with a high-pressure level. It negatively affects the liver, brain, and heart. It has been observed in many individuals that the blood pressure level improves after a reduction in alcohol consumption. Alcohol is measured in units. The recommendations are no more than 14 units of alcohol a week, 1 UNIT OF ALCOHOL is:½ pint of brewagea small glass of wine (100ml)6. Stay physically activeBeing physically active is one of the foremost necessary necessary steps in the management of high blood pressure levels. It conjointly helps to scale back your overall risk of cardiovascular disease. It is necessary to aim for a minimum of 150 minutes of moderate-intensity aerobic activity per week. A way of achieving this can be 30 minutes of brisk walk 5 days per week.Tips for staying physically active:Use the steps rather than taking the elevator.Get off the bus one or 2 stops earlier.Park your automobile at the end of the parking area.Remember to do any activity that leaves you sweating and slightly out of breath is nice.7. Try and manage your stressAnxiety and stress might raise your pressure level in the short term. This is a standard response and healthy blood vessels can deal with these changes. However, if your pressure level is raised for long periods of your time owing to continuous stress, this can eventually harm the walls of your arteries. Relaxation exercises will facilitate unleashing brain chemicals that act as your body’s natural brain tranquilizers, serving to lower pressure levels, pulse rate, and anxiety levels.
More detailsPublished - Sat, 06 Aug 2022

Created by - Dr. Prashant Raj
Everything You Need to know about Low Blood Pressure
The normal blood pressure reading is often between 90/60 and 120/80 millimetres of mercury (mm Hg) A healthy blood pressure reading for your body is predicated on your: o Medical historyo Ageo Overall health conditionYour doctor might diagnose you with low blood pressure if your reading is beneath 90/60 mmHg and you may experience symptoms such as: o Blurry Visiono Confusion/Trouble Concentratingo Dizzinesso Faintingo Light-Headednesso Nausea /Vomitingo Weakness Seek immediate treatment if you have: o A fast pulseo Shallow respiratory rateo Cold SkinThese symptoms might indicate shock, which could be a medical emergency. Low Blood pressure can occur due to various causes, including: o The sudden change in positiono Anaemiao Autonomic system disorderso Dehydrationo Abnormal diet [eating a heavy mealo Endocrine disorderso Anaphylaxiso Extreme blood losso Heart attack or cardiopathyo Low glucoseo Certain medicationso Pregnancyo Severe infectiono Stresso Thyroid conditionso Vigorous exerciseo Neurological diseases like Parkinson’s WHAT TO EAT Eat a healthy and balanced diet, however, if blood pressure becomes low frequently, you can try these tips and consume: o Have More fluids: Dehydration decreases blood volume, making your blood pressure drop Staying hydrated is very necessary, especially after strenuous activity or exercise.o Take Foods high in B-12 and folate: Insufficient nutrition of B-12 can cause anaemia, which might cause low blood pressure state and fatigue. B-12-rich foods high include eggs, fortified cereals, animal meats, and biologically processed yeast. Samples of folate-rich foods embody asparagus, beans, lentils, citrus fruits, leafed greens, eggs, and liver. o Salt. Salty foods increase the BLOOD PRESSURE, so take soup, smoke-dried fish, cheese, preserved things, and olives. o Caffeine. Caffeinated tea might quickly spike BLOOD PRESSURE by stimulating the vascular system and boosting your vital sign. Tips for avoiding low blood pressure o Talk to your dietician to incorporate healthy foods into your dieto If you think you have anaemia, make sure to get tested and start consuming iron-rich foods. o Here are several alternative changes you can make in your diet to assist raise your blood pressure: o Eat tiny meals a lot often. Massive meals might cause a lot of dramatic drops in blood pressure levels, as your body works tougher to digest larger meals. o Consume more water and less alcohol as dehydration lowers the BP o If you exercise outdoors in extreme heat, take frequent breaks and drink plenty of fluids o Avoid spending the long duration of your time in saunas, hot tubs, and steam rooms which might cause dehydration. o Change your body positions (like standing up) slowly. o Avoid prolonged bed rest. o Wear compression stockings, that facilitate blood travel upward from your legs and feet. Low BLOOD PRESSURE levels and PREGNANCY o Low blood pressure is quite common throughout the primary twenty-four weeks of pregnancy state o The vascular system starts to expand, and hormone changes cause your blood vessels to dilate. o If you experience the LOW BP state and associated symptoms in pregnancy, let your OB-GYN know as you may need extra throughout now. o Pregnancy-related low BP typically goes away shortly within the pregnancy condition or shortly when delivery. Talk to your health care provider about your overall activity level and dietary habits to see what changes, if any, you ought to make to rectify derangements in blood pressure.
More detailsPublished - Mon, 08 Aug 2022

Created by - Dr. Prashant Raj
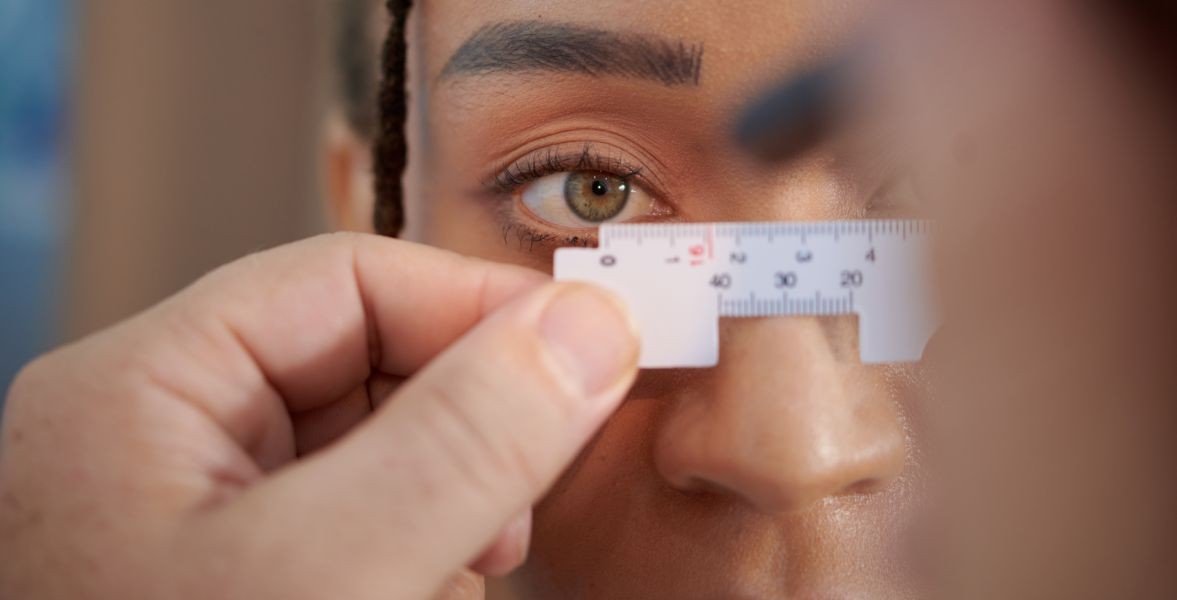
HOW TO EXAMINE EYE PROBLEMS
1. Evaluation of visual acuity is analogous to the evaluation of a patient’s vital signs during a general physical examination.a) Snellen eye chart: The patient is asked to read the chart from a distance of 20 feet.b) Finger test: The examiner should hold up his or her hand three feet away from the patient if the patient is unable to see the chart, and the patient should be asked to count the fingers.c) Motion and light perception— Motion: The examiner should wave his or her hand in front of the patient and inquire if they can "see hand motion" if the patient is unable to count fingers at a distance of three feet.— Light: The patient should also be asked if he or she can perceive light.— Peripheral vision: The patient’s peripheral vision should be checked and documented.2. Inspection of the soft tissuesa) The brows, eyelashes, and eyelids are evaluated for swelling, redness, discharge, or abnormal appearance.b) The conjunctivae are inspected for redness, infection, papillae, follicles, or discharge.3. Inspection of the pupilsa) Appearance: The size and shape of the pupils should be evaluated.b) Reaction to light: Both direct and consensual constriction should be evaluated.c) Accommodation: The patient is asked to watch the examiner’s finger as the examiner brings his or her finger toward the patient’s nose. The patient’s eyes should converge, and the pupils should constrict.4. Evaluation of extraocular motion: The six eye movements are controlled by three cranial nerves and six muscles.EYE MOVEMENTS MovementResponsible MuscleInnervationAdduction—Medial rectus—Inferior rectus—Cranial nerve III—Cranial nerve IIIAdduction— Lateral rectus— Inferior oblique— Superior rectus— Superior oblique—Cranial nerve VI—Cranial nerve III—Cranial nerve III—Cranial nerve IVElevation—Superior rectus—Inferior oblique—Cranial nerve III—Cranial nerve IIIDepression—Inferior rectus—Superior oblique—Cranial nerve III—Cranial nerve IVIntorsion—Superior oblique—Superior rectus—Cranial nerve IV—Cranial nerve IIIExtorsion—Inferior oblique—Inferior rectus—Cranial nerve III—Cranial nerve III5. Inspection of the cornea: The cornea should be inspected for clarity and smoothness. If injury to the cornea is suspected, a fluorescein stain should be placed in the eye and then the cornea should be examined for abrasions using a slit lamp under cobalt blue light.6. Inspection of the iris: The iris should be examined for any irregularity.7. Examination of the fundus is performed with an ophthalmoscope and is best accomplished after instilling a mydriatic (e.g., tropicamide 0.5%) to dilate the pupil.a) The optic disc is inspected for cupping, inflammation, and edema.b) The retina is inspected for abnormalities (e.g., hemorrhages, exudates, cotton wool spots).c) The arteries and veins are inspected for arteriovenous nicking, copper wiring, and engorgement or paucity of blood.8. Evaluation of intraocular pressure: A tonometer should be used to record the pressures in both eyes.
More detailsPublished - Mon, 08 Aug 2022
Created by - Dr. Prashant Raj
WHAT IS ANGLE-CLOSURE GLAUCOMA?
Angle-closure glaucoma, also known as closed-angle glaucoma, manifests as a forward bulge of the iris that narrows or obstructs the drainage angle between the cornea and iris. As a result, the eye's pressure rises and fluid cannot flow through it.PATHOGENESIS: Angle-closure glaucoma develops when the iris moves forward, obstructing the aqueous humor's ability to exit the eye through the trabecular meshwork. The pressure inside the eye keeps rising which could lead to damage to the optic nerve. The damaged optic nerve can cause blindness if it is not treated.PREDISPOSING FACTORS: African Americans, Asians, and women are at increased risk.CLINICAL FEATURES: The presentation may be chronic or acute.1. Symptomsa) Chronic angle closure glaucoma: Patients may be asymptomatic, or they may report a dull ache and blurred vision.b) Acute angle closure glaucoma: Patients report severe ocular pain, blurred vision, seeing halos around lights, lacrimation, nausea, vomiting, and headache.2. Physical examination findings vary according to presentation.a) Chronic angle closure glaucoma: The patient’s pupils are normal. The intraocular pressure is normal to elevated, and the cup: disc ratio is increased.b) Acute angle closure glaucoma is characterized by lid edema, conjunctival hyperemia, and circumcorneal injection.— The cornea appears cloudy as the result of microcystic edema.— The anterior chamber is shallow and cell, and flare (i.e., hazy fluid), secondary to an inflammatory reaction, is noted on slit-lamp examination.— The pupil is midsized, fixed, and often ovoid.— The intraocular pressure is markedly elevated.DIFFERENTIAL DIAGNOSES include anterior uveitis, miotic-induced glaucoma, neovascular glaucoma, and traumatic glaucoma.EVALUATION: The diagnosis is usually based on the clinical scenario.THERAPY1. Chronic angle closure glaucoma is treated with topical medications, peripheral iridectomy, or laser iridotomy on an outpatient basis.2. Acute angle closure glaucoma is an emergency. The main goal of treatment is to reduce the intraocular pressure (Given below).Pharmacologic Management of Acute Angle Closure Glaucoma1. Hyperosmotic agents are used to drawing fluid back into the blood by increasing the osmolarity of the blood. These agents must be used with caution in patients with congestive heart failure or renal failure.a) Oral agents include 50% glycerin (0.1 to 0.15 g/kg) or isosorbide.b) Intravenous agents include mannitol 20% (1 to 2 g/kg over 45 minutes).2. Carbonic anhydrase inhibitors are used to reduce the production of aqueous humor by the ciliary body. Acetazolamide (500 mg) is administered intravenously, followed by 500 mg orally, and then 250 mg orally every 6 hours.3. Beta Blockers increase aqueous outflow. Timolol 0.5% (one drop every 12 hours)4. Miotics constrict the pupil and increase the flow of aqueous humor through the trabecular meshwork. Pilocarpine 2% to 4% solution (one drop) is the agent of choice, except in the setting of recent eye surgery.5. Corticosteroids are used to reduce inflammation. Prednisolone acetate 1% (one drop every 4 to 6 hours) is the agent of choice.6. Antiemetics should be used to control nausea and vomiting, as this can increase intraocular pressure.DISPOSITION1. Chronic angle closure glaucoma: Regular eye examinations by an ophthalmologist are needed for proper management and care.2. Acute angle closure glaucoma: An Ophthalmologist should be consulted upon recognition of the condition for further management.
More detailsPublished - Tue, 09 Aug 2022

Created by - Dr. Prashant Raj
How to manage a patient with Knife Cut
Accidental knife cuts referred to as lacerations are seldom life-threatening. If someone sustains such injuries then the goals are to: · Minimize infection· Promote healing· Decrease the necessity for surgical intervention The first factor you ought to do with any laceration is calm the victim and, once attainable, elevate the affected part of the body higher than the level of the victim’s heart. Wear first-aid gloves and protect your eyes. The next step is to stop the blood. This can be best accomplished by applying direct and constant pressure to the wound by employing a wadded sterile compress, cloth, or direct hand-to-wound contact (that’s why you “gloved up”) if needed. Hold pressure for a full ten to fifteen minutes. If you still see the blood oozing out, then the clock resets and you got yourself another ten to fifteen minutes. Then consider a pressure bandage, compression bandage or alternative additional extreme measures. With the blood stopped, take a look and in-depth inspect the injury. Check the pulses around the wound; they must be sturdy and regular. The tissue surrounding the wound ought to be warm and pink with no loss of sensation, and all the motor activities need to be intact. In general, any variations from these needs to be taken seriously, and call for immediate medical attention. Now, you've got to scrub/irrigate the wound to forestall infection. The simplest irrigants are traditional saline and sterile water. Avoid the use of iodine (Betadine), lotion, and oxide, which may cause additional tissue harm. The irrigation stream needs to have enough force behind it to dislodge any foreign material while not injuring the tissue beneath and you've got to use caution to not push harmful material deeper into the wound. The goal isn't to soak the wound but to scrub it. Use a minimum of one liter of irrigation fluid to scrub every wound. When irrigation is done, bandage a laceration with non-adherent dressings made of materials such as Telfa, Xeroform, Adaptic, and Aquaphor. You can apply an antiseptic ointment like an antibiotic to the surface of the wound before seeking proper medical care Be sure to stay up-to-date on your tetanus shots and seek skilled medical attention as early as possible!
More detailsPublished - Tue, 09 Aug 2022

Created by - Dr. Prashant Raj
ANAPHYLAXIS AND ITS CLINICAL FEATURES
1. The acute, potentially fatal illness known as anaphylaxis is brought on by the release of chemical mediators from mast cells and basophils. The primary preformed chemical mediator is histamine. Proteoglycans, enzymes in the Hageman factor pathway, neutrophil chemotactic factor, and eosinophil chemotactic factor are more examples.2. Anaphylactic versus anaphylactoid reactionsa) Unlike anaphylactoid reactions, which happen through a variety of pathways and directly degrade mast cells, anaphylactic reactions entail antibody-antigen interactions mediated by immunoglobulin E (IgE).i) Anaphylaxis— In IgE-mediated reactions, the antigen has already been exposed, specific IgE has been produced by plasma cells, and the IgE has been able to bind to receptor sites on mast cells and basophils. This results in the release of preformed mediators, particularly histamine, which triggers a chain of subsequent events that end in anaphylaxis.— One-third of all occurrences of anaphylaxis are caused by food, and other causes include antibiotics, foreign proteins (such as streptokinase), hymenopteran venom, and preservatives. Idiopathic conditions make up about one-third of all cases.ii) Anaphylactoid reactions—Anaphylactoid reactions occur via mechanisms that do not involve IgE. The sequence of events involves the direct release of mediators from mast cells and basophils.— Causes of anaphylactoid reactions include human plasma and blood products, direct histamine releasers (e.g., opiates, curare, dextran, radiocontrast media), and miscellaneous agents and processes, such as exercise, physical factors, vibration, nonsteroidal anti-inflammatory drugs (NSAIDs), and mastocytosis.b) Anaphylactic and anaphylactoid reactions are clinically the same because comparable mediators produce similar target organ sequelae. Treatment for both reactions is directed at the end-organ signs and is the same. Because of these similarities, the term anaphylaxis will be used to encompass both IgE and non-IgE reactions.CLINICAL FEATURES 1. Symptoms are most likely to occur minutes after exposure to the triggering agent but may occur in seconds to a few hours. Early or subtle signs and symptoms of anaphylaxis include cutaneous flushing, pruritus, voice change, and a sense of impending doom. Usually, the later the symptoms occur, the less severe the reaction.2. Clinical findings prominently involve the skin (urticaria), the upper airways (laryngeal edema, hoarseness, stridor), the lower airways (bronchospasm), and the cardiovascular system (hypotension, vasodilation, dysrhythmia, myocardial infarction [MI]), and the gastrointestinal system (abdominal cramps).3. Death may occur from respiratory causes (70%) or cardiovascular causes (25%). (Autopsy findings include acute pulmonary hyperinflation, laryngeal edema, visceral congestion, pulmonary edema, intra-alveolar hemorrhage, urticaria/angioedema, and MI.)Clinical Manifestations of AnaphylaxisOrgan SystemReaction Cutaneous - Diaphoresis- Flushing- Pruritus- Piloerection- Urticaria- Angioedema Head, ears, eyes, nose, and throat-Conjunctivitis-Metallic taste-Hoarseness-Rhinorrhea/nasal congestion-StridorPulmonary- Dyspnea- Cough- Tachypnea- Wheezing Cardiovascular- Tachycardia- Dysrhythmia- HypotensionGastrointestinal-Abdominal cramps-Diarrhea Nausea and vomitingNeurologic- Altered mental status- Dizziness- SeizureDIFFERENTIAL DIAGNOSES: The diagnosis of anaphylaxis is generally readily apparent based on history and clinical findings but may sometimes be confused with overlapping or other distinct entities.Differential diagnosis involves the following:1. Judging whether the symptoms and signs represent a simple allergic or pseudoallergic reaction (e.g., asthma exacerbation, urticaria), as opposed to anaphylaxis2. Considering whether some of the symptoms and signs represent a secondary process (e.g., MI). 3. Determining if a completely different type of problem could be occurring (e.g., drug intoxication, hypovolemic shock).
More detailsPublished - Wed, 10 Aug 2022

Created by - Dr. Prashant Raj
Fever – Cause, Symptoms & Treatment
Fever is defined as a state of a temporary rise in body temperature attributed to a response from the body's immune system. Whenever any foreign invaders like viruses, bacteria, fungi, drugs, or different toxins enter the body, the immune system responds immediately which can sometimes cause fever.Children below 3 months of age with a higher-than-normal 97.52 F temperature OR 100.4 F (38.0 C) or above needs to be seen by a skilled health care expert. They’ll be quite sick and do not show any signs or symptoms besides a fever. Acetaminophen (Tylenol and others) and Motrin (Advil, Motrin) are used to treat a fever. Pain pills aren't recommended in children to regulate fever.The prognosis depends upon the cause of the fever. Most cases of fever are usually resolved with treatment of symptoms. Someone, who is on immune suppressant drugs or has a history of cancer, AIDS, or different serious unwellness, like cardiovascular disease or chronic disease, should immediately take treatment if a fever develops.Fever may be a routine symptom in infants and youngsters. It’s a standard reaction to extreme heat or viral/bacterial infection, but that does not mean that the fever should be neglected. However, if the kid is otherwise doing well, treating the fever with over-the-counter (OTC) medicines like Tempra (Tylenol and lots of others) or Motrin (Advil, Motrin, and lots of others) is also all that's required.Causes of Fever -• The rise in body temperature is attributed to a response from the body's immune system due to any foreign invaders like viruses, bacteria, fungi, drugs, or different toxins.• These foreign invaders induce fever-producing substances (called pyrogens), that trigger the body's reactionSymptomsA fever will cause someone to feel uncomfortable. Signs and symptoms of a fever embrace the following:• Temperature more than a 100.4 F (38 C) in adults and youngsters• Shivering, shaking, and chills• Aching muscles and joints /body aches• Headache• Intermittent sweats or excessive sweating• Rapid heart rate and/or palpitations• Skin flushing or hot skin• Feeling faint, dizzy, or lightheaded• Eye pain or sore eyes• Weakness• Loss of appetite• Fussiness (in youngsters and toddlers)TreatmentA fever isn't unremarkably harmful on its own. Most fevers go away on their own in some hours to days as your body defeats the infection.Home remedies for fever:- • Stay hydrated by drinking many fluids, such as water, juice, and soup• Eat lightweight foods that are easy to digest.• Rest and take a proper diet.• Use a cool compress, sort of a damp towel.• Dress in lightweight, and lose clothingOver-the-counter medications will facilitate ease your fever and symptoms, like headaches and muscle pain:• ibuprofen (Advil, Motrin)• acetaminophen (Tylenol )•naproxen (Aleve, Naprosyn)You may need to take treatment from your doctor for additional serious causes of a fever. The treatment depends on the cause. Your doctor might give medications to treat serious infections:• Antibiotics• Antivirals• Antifungal
More detailsPublished - Wed, 10 Aug 2022

Created by - Dr. Prashant Raj
EVALUATION AND TREATMENT OF ANAPHYLAXIS
For making the diagnosis and determining the intensity of the reaction to formulate the management strategy, the history and physical examination are essential.1. Patient historya) The cause of the anaphylaxis should be determined.— Antibiotics including penicillin are a major source of negative medication responses. The majority of responses happen after parenteral administration as opposed to oral.— Radiocontrast media cause anaphylactoid reactions at a rate of 0.22% for ionic (high osmolar) agents. The risk of death has been estimated to be 1 in 10,000 (0.01%). Nonionic (low osmolar) agents cause anaphylactoid reactions at a rate of 0.04%.— Lidocaine and other local anesthetics rarely cause true allergic reactions, but many patients report “allergy to ‘caines’” because a variety of nonallergic reactions are associated with its administration.b) The route and timing of exposure should be ascertained. The route may be by injection, ingestion, inhalation, or cutaneous absorption.c) Other details that may be crucial for the evaluation and management of the case include previous reactions to the same substance and the severity of those reactions, underlying medical conditions like cardiovascular disease or pulmonary disease, current medications like beta-blockers, antihistamines, and corticosteroids, as well as medication allergies.2. Laboratory testing (see Table)DIFFERENTIAL DIAGNOSES OF ANAPHYLAXIS Asthma exacerbationHypovolemic shock or sepsisCarcinoid syndromeMastocytosisCerebrovascular accident Myocardial infarctionDrug intoxicationPulmonary embolus Hereditary angioedemaSeizure disorderHyperventilationUrticarial syndromeHypoglycemiaVasovagal syncope Laryngeal foreign bodyTrauma to larynx3. Radiography: A chest radiograph may reveal hyperinflation or atelectasis.THERAPY1. Prompt intervention is vital: a) Antigen exposure needs to be stopped, and vital signs need to be watched. At the first sign of the reaction, any intravenous antigen infusion should have been discontinued, and any topical medications should have been removed. Gastric lavage should be taken into consideration if the agent was recently consumed. b) Epinephrine is administered to prevent mediator release. It relaxes laryngeal and bronchial smooth muscle and supports blood pressure.i) Side effects: Epinephrine may cause vomiting, hypertension, tremor, and tachydysrhythmia.ii) Possible contraindications include cardiac ischemia, severe hypertension, and pregnancy. Glucagon can be substituted if epinephrine is contraindicated.iii) Dosage and administration— Epinephrine 0.1% (1:1,000 preparation). In patients with stable vital signs, epinephrine 0.1% is given subcutaneously or intramuscularly every 15 minutes as required. The dosage is 0.3 to 0.5 mL for adults and 0.01 mg/kg for children.— Epinephrine 0.01% (1:10,000 preparation) is administered intravenously when there is significant airway compromise or shock. For adults, the dosage is 1 to 3 mL, administered slowly intravenously (or diluted in normal saline to 10 mL and administered via an endotracheal tube). Children receive 0.1 mg/kg by slow intravenous infusion.c) Stabilization of airway, breathing, and circulation (ABCs)i) The airway should be observed closely and supported as needed with endotracheal intubation or cricothyrotomy.ii) High-flow oxygen should be administered.iii) Blood pressure should be supported by placing the patient in a recumbent position, infusing intravenous fluids, and, if necessary, administering a continuous infusion of epinephrine.d) Treatment of bronchospasm is with Beta agonists or nebulized epinephrinee) Histamine receptor blockadei) Histamine-1 receptors should be blocked with an antihistamine such as diphenhydramine (1 to 2 mg/kg intravenously, up to a total dose of 50 mg, initially and every 6 to 8 hours as needed, for adults and children).ii) Histamine-2 receptors. Blocking the histamine-2 receptors with an agent such as cimetidine or ranitidine may also be advantageous.f) Prevention of late-phase reactions: A corticosteroid (e.g., prednisolone, 1 to 2 mg/kg intravenously every 6 hours until conversion to oral medication) should be administered intravenously in an attempt to abort late-phase reactions.g) Treatment of refractory anaphylaxis: In the presence of β- blockade, anaphylaxis may be particularly refractory to treatment, and glucagon (0.05 mg/kg administered as an intravenous bolus, followed by an infusion at a rate of 0.07 mg/kg/hour) may need to be employed.2. Late-phase reactions may occur in the ensuing 6 to 48 hours. The treatment strategy for a late-phase reaction is the same as that for an initial reaction.
More detailsPublished - Thu, 11 Aug 2022

Created by - Dr. Prashant Raj
DISPOSITION AND PREVENTION OF ANAPHYLAXIS
DISCHARGE: Patients who exhibit a modest reaction upon presentation, respond favorably to treatment, remain symptom-free for 4 to 6 hours following initial treatment, are trustworthy, and have strong support networks may be eligible for discharge home.a) It should be advised to these patients to take oral antihistamines and steroid medicine for a few days and to immediately see the emergency department (ED) if any symptoms start to reappear. They should be instructed to stay away from the alleged agent or agents and to follow up with their family doctor.b) Patients with conditions such as Hymenoptera -sting anaphylaxis need instructions regarding the acquisition of a medical alert bracelet, tag, or card; provision of epinephrine auto-injector (e.g., EpiPen [Mylan]) so that early treatment may be self-initiated in the event of another episode of anaphylaxis, and referral to an allergist.ADMISSION: Patients need to be admitted to the hospital and placed in an intensive care unit if they have bronchospasm, hypotension, cardiovascular issues, or changed mental status. Although this is becoming less frequent, patients who get treatment for an initially severe anaphylactic reaction but who quickly become asymptomatic may be admitted to the hospital.PREVENTION OF ANAPHYLAXIS1. Allergic reactions should be documented in the medical record.2. Inquiries regarding the history of allergy should be made before administering medication, and any worrisome report should be heeded.3. When possible, highly allergenic drugs should be given orally rather than parenterally. If an injection is given, the patient should be observed for 20 to 30 minutes.4. Desensitization may be feasible and indicated for certain agents such as penicillin, Hymenoptera venom, and aspirin (See table).Local Anesthetic Chemical GroupsGroup I: Esters(a) Group II: Amides(b) Others(c) BenzocaineBupivacaineDibucaineProcaine LidocaineDyclonineProparacaineMepivacainePramoxine TetracainePrilocaine(a) May cross-react.(b) Unlikely to cross-react.(c) For mucous membrane administration.
More detailsPublished - Sat, 13 Aug 2022
Search
Popular categories
Latest blogs
All you need to know about Syphilis
Tue, 15 Nov 2022
What is Pemphigus Vulgaris?
Tue, 15 Nov 2022

Know about Scorpion Stings
Sat, 12 Nov 2022
Write a public review