
Created by - Dr. Prashant Raj
How to Deal with Otitis Externa
1. Otitis externa is inflammation of the external auditory canal and /or the auricle.2. Necrotizing (malignant) otitis externa is a severe form of otitis externa that involves the infection and inflammation of surrounding tissues. It is almost always caused by Pseudomonas and occurs in patients with diabetes and other debilitating diseases.ETIOLOGYOtitis externa is usually caused by a bacterial infection (most often Pseudomonas , Staphylococcus, Streptococcus, or a gram-negative rod). Other, less common causes include fungal infection (most commonly Aspergillus) and eczema.PREDISPOSING FACTORS — Trauma to the epithelium— Swimming— Hot, humid weather— Cotton ear swabs— The use of a hearing aidCLINICAL FEATURES1. Symptoms include otalgia, pruritus, plugging of the ear, and decreased hearing.2. Physical examination findingsa) The canal is erythematous, often with a purulent discharge.b) The preauricular lymph nodes may be swollen.c) When the tragus pinna is pulled to open the canal for visualization, there is often pain.DIFFERENTIAL DIAGNOSES— Eczematous otitis externa— Necrotizing otitis externa— Otitis media— Mastoiditis— A foreign bodyEVALUATIONThe results of the physical examination are typically used to make a diagnosis. The only time additional testing is warranted is if necrotizing otitis externa is suspected; in this situation, a CT scan to evaluate the deep tissues may be appropriate.THERAPY1. Cleansing: The canal should be cleaned of debris by gentle irrigation with tepid water or 2% acetic acid solution (vinegar).2. Antimicrobial therapya) Uncomplicated otitis externa: A topical antibiotic with steroids (e.g., polymyxin B otic suspension) should be instilled in the ear (four drops three times daily for 10 days).b) Necrotizing external otitis media is treated intravenously with ciprofloxacin (400 mg every 12 hours) and in this instance also used in pediatric patients.c) Fungal infection: Amphotericin B should be used in consultation with an infectious disease specialist.DISPOSITIONPatients with uncomplicated otitis externa can be sent home with instructions to follow up with a primary care physician in 3 to 5 days. The ear should be kept clean and dry, and the patient should be educated about minimizing the use of cotton swabs. Patients with necrotizing otitis externa must be admitted for intravenous antibiotic therapy.
More detailsPublished - Tue, 18 Oct 2022

Created by - Dr. Prashant Raj
Smoking - An Unhealthy Life
Smoking hurts the digestive system of our body slowly and gradually. It has been observed that peptic ulcer is commonly found in smokers as compared to non-smokers. In addition to this, smoking makes certain chronic conditions like diabetes, tougher to treat. Smoking increases the danger of developing inflammatory bowel disease, gallstones, and many types of cancers [Head & neck, Lung, stomach, pancreas, and colon].The stomach makes acidic juices that assist you digest food. If these juices flow backward into your esophagus or food pipe, they can cause heartburn due to a condition known as Oesophageal reflux unwellness (GERD). The esophagus is protected against these acids by the lower esophageal sphincter which prevents the reflux of acid from the stomach to the esophagus. However, smoking weakens the muscles of this sphincter, thereby permitting the reverse flow of acid. Ulcers are painful sores within the lining of the stomach or the start of the small bowel. Ulcers heal fast if you stop smoking. Smoking conjointly raises the danger of infection from Helicobacter pylori. This is a bacterium unremarkably associated with ulcers.The liver ordinarily filters alcohol and other toxins out of your blood. however, smoking limits your liver’s ability to get rid of these toxins from your body. If the liver isn’t operating as well as it ought to, it's going to not be able to metabolize medications well. Studies have shown that once smoking is combined with drinking an excessive amount of alcohol, it makes the disease worse.Smoking is one of the foremost risk factors for carcinoma. carcinoma is the second leading reason behind cancer deaths. Routine screenings, like an endoscopy, can pick the premalignant growth such as polyps within the lining of the colon. Some analysis suggests that smoking also increases the danger of developing gallstones.
More detailsPublished - Tue, 18 Oct 2022

Created by - Dr. Prashant Raj
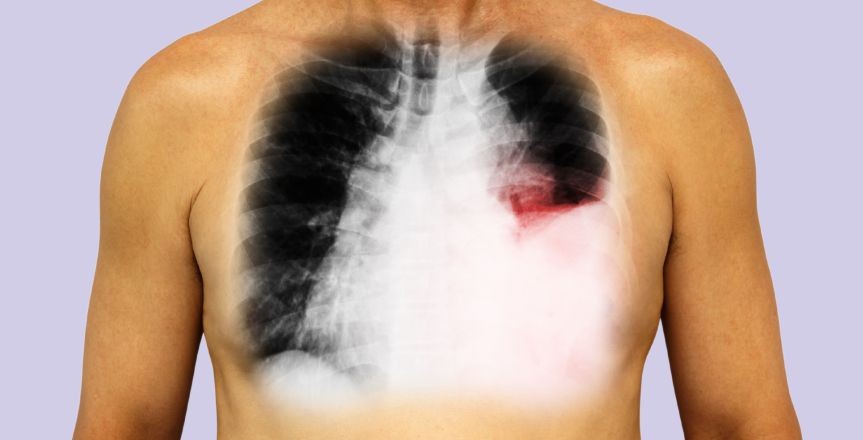
Noncardiogenic pneumonic edema
Noncardiogenic pulmonary oedema is an illness that leads to acute hypoxia secondary to a fast deterioration in respiratory function. The illness has multiple etiologies, all of that need prompt recognition and intervention. The permeability of the alveolar-capillary membrane is increased which leads to the increased leak of protein and water in the alveolar space causing an increase of intra-alveolar fluid, thereby increasing pulmonary vascular resistance, intrapulmonary shunt, and hypoxemia. This will cause a marked reduction in compliance of Lung. To differentiate from cardiogenic pulmonary oedema, pneumonic capillary wedge pressure isn't elevated. This is often necessary to differentiate because the management of both conditions is different. Pulmonary oedema that's not caused by hyperbolic pressures within the heart is termed noncardiogenic pneumonic oedema.Causes of noncardiogenic Pulmonary oedema include:o Acute respiratory distress syndrome (ARDS). This serious disorder happens once the lungs suddenly fill with fluid. several conditions will cause respiratory illness, as well as severe injury (trauma), and widespread infection (sepsis), respiratory illness.o Drug reactions or side effects of several medications — starting from acetylsalicylic acid to medication like opiate and cocaine — are best known to cause pulmonary oedema.o Blood clot in the lungs (pulmonary embolism). A clot moving from the blood vessels of the legs to the lungs can cause pulmonary oedema.o Exposure to some toxins. Exposure to some toxins or aspirating some refluxed abdomen contents may cause intense irritation of the tiny airways and air sacs, leading to fluid build-up.o High altitudes. Pulmonary oedema has been seen in mountain climbers, skiers, hikers and others who trip high elevations, typically around 8,000 feet. High altitude Pulmonary oedema (HAPE) typically happens in those that do not take the times or weeks necessary to become accustomed to the elevation. however, people that live at high altitudes will get HAPE with no elevation amendment if they need a respiratory disorder.o Near drowning episodes in water can cause fluid build-up within the lungs.o Negative pressure Pulmonary oedema. A blocked higher airway causes negative pressure within the lungs from attempting to breathe through the blockage. With treatment, most patients recover within 24 hrs with this type of Pulmonary oedema.o Nervous system conditions or surgeries. Pulmonary oedema occurs after a head injury, seizure or surgery.o Smoke inhalation. Smoke from certain chemicals can harm the membrane between the air sacs and also the capillaries. This harm permits fluid to enter the lungs.o Transfusion-related respiratory organ injury. Blood transfusions might cause fluid overload resulting in Pulmonary oedema.o Viral sicknesses. Viruses like the hantavirus can cause Pulmonary oedema.
More detailsPublished - Wed, 19 Oct 2022

Created by - Dr. Prashant Raj
Sinus Infection (Sinusitis): Causes, Symptoms, Evaluation & Treatment
Sinusitis is an inflammation of the paranasal (ethmoid, frontal, maxillary, or sphenoid) sinuses. It is classified as acute or chronic, depending on how long the infection has been present.ETIOLOGY AND PATHOGENESISSinusitis occurs when pus is trapped in the sinus and is unable to drain completely through the Ostia into the nasal cavity.a) Bacterial causes include H. influenzae, S. pneumoniae, streptococci, and M. catarrhalis.b) Fungal causes are most common in patients with diabetes. Mucormycosis is particularly life-threatening.PREDISPOSING FACTORS— Chronic nasal edema— Nasal polyps— Nasal allergies— Preceding upper respiratory tract infection— Upper tooth abscessCLINICAL FEATURES1. Symptomsa) Pain: Nasal congestion increases the pressure in the sinus, leading to pain that often worsens when the patient bends over. Patients may complain of a headache. Facial pain often corresponds to the affected sinus:— Cheeks and upper teeth—maxillary sinus— Eyebrow area—frontal sinus— Eyes or behind the eyes—ethmoid sinusb) Generalized malaise and periorbital edema are common complaints.c) Nasal discharge is often blood-tinged and purulent. A postnasal drip may cause coughing and a sore throat.2. Physical examination findingsa) Fever is often present in acute sinusitis but is rare in chronic sinusitis.b) Tenderness to percussion may be present over the affected sinus.c) The opacity of the affected sinus may be evident during transillumination. A negative transillumination does not rule out sinusitis because the test is only positive when the sinusitis is advanced.DIFFERENTIAL DIAGNOSES— Viral rhinitis— Allergic rhinitis— Vasomotor rhinitis— Tumors— Foreign bodies— Wegener granulomatosisEVALUATION1. Laboratory studies: Typically not indicated. In acute sinusitis, a CBC may reveal an elevated white blood cell count.2. Imaging studiesa) Radiographs: Plain sinus films may reveal air-fluid levels, cloudiness, or thickening of the sinus mucosa.b) CT scans may identify an underlying predisposing anatomic condition (e.g., abnormally narrowed outlets, tumorous or cystic obstructions).THERAPY1. Supportive measuresa) An effort should be made to avoid air-borne irritants (e.g., smoke, pollen).b) Although steam inhalation and environmental humidification are useful adjuncts, aggressive systemic rehydration is essential to mobilize and prevent reaccumulation of the thickened secretions.c) Analgesics, decongestants, antihistamines, and steroids may also be helpful.2. Antibiotic therapy: Not indicated in most cases. If determined necessary, acceptable regimens include:a) Amoxicillin clavulanate (500 mg three times daily for 2 to 3 weeks)b) Doxycycline (100 mg twice a day for 10 days)3. Surgery: Surgical drainage of the sinus may be indicated if medical treatment fails. Surgery may also be indicated to correct underlying anatomic defects.DISPOSITIONAll patients diagnosed with sinusitis should be followed up until clinically cured.1. Discharge: In the absence of complications (e.g., orbital cellulitis, osteomyelitis, septic cavernous thrombosis, contiguous spread to involve the nervous system), patients can be sent home with instructions to follow up in 1 to 2 days.2. Admission is indicated for extremely ill patients, patients with orbital edema, and patients with nuchal rigidity or altered mental status.
More detailsPublished - Wed, 19 Oct 2022

Created by - Dr. Prashant Raj
Peritonsillar Cellulitis and Peritonsillar Abscess
When acute bacterial tonsillitis is present, there is always the possibility of spreading to surrounding tissue in the pharynx.1. Peritonsillar cellulitis is an infection that has spread to the surrounding area, causing inflammation and edema in the peritonsillar area.2. Peritonsillar abscess is present when the infection progresses to form an abscess or collection of pus in the pharyngeal pillar.ETIOLOGYThe most common cause is β-hemolytic Streptococcus, but often the infection is polymicrobial, involving Streptococcus pneumoniae, H. influenzae, and Staphylococcus, as well as anaerobes such as Bacteroides fragilis.COMPLICATIONSLocal extension of the cellulitis or abscess can lead to more serious conditions:a) Extension of the abscess into contiguous neck spaces, including the retropharynx, subglossal spaces, and mediastinumb) Erosion into the carotid artery, leading to life-threatening hemorrhage, or into the internal jugular vein, leading to septic thrombosisCLINICAL FEATURES1. Symptomsa) The classic features of tonsillitis—fever, sore throat, and odynophagia —are present for 2 to 3 days. The throat pain localizes to one side. The patient may drool because of an inability to swallow.b) The patient may also complain of dysphagia, dysphonia, and referred pain to the ear.2. Physical examination findingsa) Trismus (spasm of the muscles of mastication) may be present and the patient may have difficulty opening the mouth.b) Marked swelling of the pharyngeal pillar displaces it downward. Pushing the uvula to the other side.— In peritonsillar cellulitis, the pillar will be soft and not as enlarged as it is in patients with a peritonsillar abscess.— In peritonsillar abscess, the pillar is larger and firm or fluctuant.DIFFERENTIAL DIAGNOSESa) Epiglottitis does occur in adults, and an absence of pharyngeal findings or the presence of stridor should warrant consideration of this diagnosis.b) If a non-infectious asymmetrical swelling is present, squamous cell carcinoma, lymphoma, a vascular lesion, or other neoplasms should be considered.c) Mononucleosis and other viral infections, as well as diphtheria, must be ruled out.EVALUATION1. Needle aspiration of the tonsillar pillar allows differentiation between cellulitis and an abscess. Failure to aspirate pus in a soft pillar will indicate cellulitis, whereas the diagnosis is peritonsillar abscess if pus can be aspirated.2. Laboratory studies are of little value in the diagnosis. However:a) In septic, dehydrated, or diabetic patients, additional workup, including a CBC, serum electrolyte panel, and a glucose level, may be appropriate.b) If mononucleosis is suspected, a monospot test may be of value.3. Imaging studies: CT scans can delineate the size and location of cellulitis/ abscess and the risk of impending airway compromise.THERAPY1. Abscess drainage: If an abscess is present, it needs to be drained.a) Needle aspiration without opening the abscess is advocated by some.b) Incision and drainage by opening the abscess with a scalpel and gently opening the space with forceps is the second option.2. Antibiotic therapya) Patients who can swallow and are not dehydrated or toxic can be administered oral antibiotics. Acceptable regimens include:— Amoxicillin-clavulanate (875 mg every 12 hours)— Clindamycin (450 mg every 6 hours)b) Dehydrated patients who are unable to swallow should receive intravenous fluids and antibiotics.— Ampicillin-sulbactam (3 g every 6 hours)— Clindamycin (600 mg every 6 hours)3. Supportive therapya) Saltwater gargles often help soothe the throat and rinse the incised pillar. Mouthwashes should be avoided because they are irritating.b) An analgesic/antipyretic agent should be prescribed.DISPOSITION1. Discharge: Patients who are discharged after initiating intramuscular or oral antibiotic therapy should be seen within 24 hours for reevaluation. These patients should be instructed to return to the ED if they experience trouble swallowing or breathing.2. Admission is required for any patient who is unable to swallow, dehydrated, toxic, or immune-compromised.3. Referral: Consultation with an ear, nose, and throat specialist should be arranged if the patient was not seen by a specialist in the ED.
More detailsPublished - Thu, 20 Oct 2022

Created by - Dr. Prashant Raj
Dental Caries (Cavities)
Cavities are tiny cracks or openings/break that permanently harm the strong enamel of your teeth. Cavities, also known as tooth decay or caries, are caused by a variety of factors, such as oral bacteria, frequent eating, drinking sugary beverages, and insufficient teeth cleaning. Dental caries (cavities) result from bacterial erosion through the enamel into the dentin and pulp.CLINICAL FEATURES1. Symptoms: The chief complaint is usually a “toothache” or jaw pain. The pain is exacerbated by hot and cold liquids or food. The tooth is often sensitive to touch as well. Pain can be referred to the jaw or ear.2. Physical examination reveals pitting of the tooth surface. Percussion of the tooth or probing of caries may elicit pain.DIFFERENTIAL DIAGNOSES 1. It includes apical abscess, periodontal abscess, and fracture of the tooth. 2. Myocardial infarction can present as tooth or jaw pain and should be considered in a patient who is short of breath or ill-appearing and in whom no caries can be readily identified.EVALUATION: Physical examination is the sole means of evaluation.THERAPY: In the ED, supportive care can be provided (e.g., analgesics, local anesthesia with a lidocaine or mepivacaine injection at the root of the tooth, and placement of dental wax in the cavity to reduce sensitivity).Disposition: Patients are discharged with instructions to see a dentist as soon as possible.
More detailsPublished - Fri, 21 Oct 2022
Created by - Dr. Prashant Raj
Pleural Effusion
The accumulation of fluid in layers in the layer between the lungs and chest cavity. A small amount of fluid is present in this cavity for lubrication during breathing, but too much accumulation can cause a problem, which is stated as pleural effusion. CausesA wide variety of things can cause a serious membrane effusion which may includeo Congestive heart failure. o Cirrhosiso Pulmonary embolismo Cancer.o Kidney diseaseo Infections: pneumonia.o Autoimmune conditions. Lupus or rheumatoid arthritis SymptomsYou may not have any symptoms in case of a small effusion, but, if there is a large or moderate-sized pleural effusion, or if there's associated inflammation. Then you may haveo Shortness of breatho Chest pain, especially during deep inhalation (This is termed pleuritic pain.)o Fevero Cough Types of pleural effusion "Transudative" and "Exudative" are the 2 main types of pleural effusions Type of Pleural Effusion Transdutaive Exudative Cause Increased pressure in the blood vessels can lead to the leaking of fluid into the pleural space The fluid buildup occurs owing to infection, injury, and the associated inflammation Conditions that can give rise to this effusion type > Congestive heart failure > Cirrhosis > kidney disease > Malnutrition > tuberculosis > cancer > inflammatory conditions, [lupus, or rheumatoid arthritis] > pneumonia
More detailsPublished - Sat, 22 Oct 2022

Created by - Dr. Prashant Raj
Encephalitis: Symptoms, Causes & Evaluation
The brain stem, cerebellum, and cerebrum are all infected by encephalitis. Encephalitis may be caused by several organisms, including HSV type 1 and arboviruses (e.g., Eastern equine encephalitis virus, Western equine encephalitis virus, St. Louis encephalitis virus, California encephalitis virus), Mycoplasma, Toxoplasma, Coccidioides, Cryptococcus, T. pallidum, Borrelia burgdorferi, Naegleria, and Mycobacterium.CLINICAL FEATURES:Symptoms are very similar to those of meningitis. An altered level of consciousness ranging from lethargy and irritability to frank obtundation and coma is common. Seizures and gait ataxia also occur. Personality change is generally a key factor to differentiate encephalitis from meningitis.DIFFERENTIAL DIAGNOSES include meningitis, brain abscess, neoplasm, trauma, subdural hematoma, subarachnoid hemorrhage, systemic lupus erythematosus, toxic encephalopathy, and metabolic encephalopathy.EVALUATION: The foundation of the diagnosis is a head CT scan and CSF analysis. The diagnosis of encephalitis is usually made by first ruling out the presence of meningitis using Gram staining, antibody titers, India ink preparations, and CSF cultures.1. CSF analysis: A CSF sample obtained via a lumbar puncture usually shows a normal glucose level, an elevated protein level, and marked pleocytosis in patients with encephalitis, but these signs are nonspecific. When HSV or Naegleria is the causative organism, an elevated CSF red blood cell count is common. Specific CSF and blood serum titers for specific encephalitides (e.g., Toxoplasmosis) are available and useful for identifying the causative agent.2. HSV polymerase chain reaction should be ordered when considering herpes encephalitis.THERAPY: Because differentiating encephalitis from meningitis is very difficult, presumptive therapy should be initiated for bacterial meningitis even before the initiation of the workup. Treatment is generally supportive. HSV is treated with acyclovir with the goal of early administration.DISPOSITION: All patients suspected of having encephalitis should be admitted to the hospital for further evaluation and treatment.
More detailsPublished - Sat, 22 Oct 2022

Created by - Dr. Prashant Raj
Brain Abscess: Risk Factors, Symptoms & Treatment
INCIDENCE: Brain abscesses are rare. The greatest incidence is seen in patients between the ages of 20 and 40 years; men are affected twice as often as women.PATHOGENESIS1. Abscesses typically develop as a result of an external infection focus.a) Brain abscesses arise from the middle ear, mastoid, and paranasal sinuses 40% of the time.b) The hematogenous spread of bacteria from remote sites causes 30% of infections.c) Thirty percent of brain abscesses have no clear cause.2. The cerebrum becomes inflamed, an abscess forms, and then it becomes encapsulated. Three major complications can cause sudden deterioration: uncal or tonsillar herniation, spontaneous hemorrhage, and rupture of the abscess into the ventricular or subarachnoid space.RISK FACTORS for brain abscess include AIDS, immunosuppression, and intravenousdrug abuse.CLINICAL FEATURES: The clinical presentation may mimic that of a brain tumor, but the presentation of an abscess usually evolves more rapidly (e.g., within days to weeks). The classic presentation is one of headache, recent seizure, low-grade fever, and a focal neurologic deficit.a) Headache is the most common symptom; it is present in 70% to 90% of affected patients.b) Focal neurologic deficits are found in 75% of patients.c) Seizures are found in 30% of patients; fever in 50% of patients.DIFFERENTIAL DIAGNOSES include a tumor, encephalitis or meningitis, cerebrovascular accident, subarachnoid hemorrhage, migraine, and an extradural abscess.EVALUATION: Cerebral inflammation develops into an abscess and then becomes encapsulated. Laboratory values are rarely helpful, although the WBC count is elevated in 30% of patients.THERAPY: Surgical intervention and antibiotic treatment are part of definitive care.1. Supportive therapy: If there are signs of increased intracranial pressure, the physician may need to elevate the bed 30 degrees, intubate the patient, and institute dexamethasone therapy (10 mg intravenously followed by 4 mg every 6 hours for adults; 0.6 mg/kg every 6 hours for children).2. Antibiotic therapy: Drugs should be selected using susceptibility testing as a basis (see table below), and therapy should be continued for 4 to 6 weeks.DISPOSITION: Patients with brain abscesses require hospital admission and immediate neurosurgical consultation.
More detailsPublished - Wed, 26 Oct 2022
Search
Popular categories
Latest blogs
All you need to know about Syphilis
Tue, 15 Nov 2022
What is Pemphigus Vulgaris?
Tue, 15 Nov 2022

Know about Scorpion Stings
Sat, 12 Nov 2022
Write a public review